Epic Integration with other healthcare software enhances interoperability. Epic API integration facilitates seamless data exchange between the EHR platform and diverse medical platforms, even if they utilize different data formats.
How does integrating Epic enhance healthcare workflows?
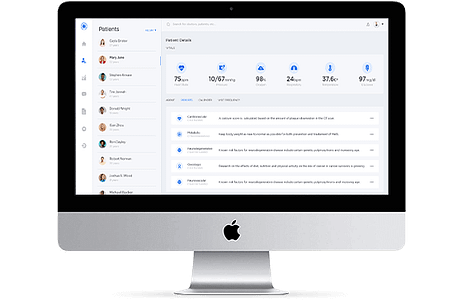
Epic integration streamlines the general operational processes in all departments within healthcare organizations. Doctors, nurses, front-office staff, and administrators can swiftly access a centralized database for their tasks with a few clicks.
This allows healthcare providers to promptly retrieve patient data and medical notes. Billers can efficiently access services, perform charge capture, and generate claims. Similarly, other team members can utilize the identical data to create discharge summaries.
What systems can seamlessly exchange data with Epic through integration?
- Electronic Health Records
- Practice management solutions
- Medical billing and coding software
- Clinical decision support system
- mHealth software
How does Epic integration improve patient care and security?
Managing gaps in patient data:
Gaps in medical information about patients raise the risk of misdiagnoses and errors in treatment. However, Epic EHR integration enables healthcare providers to access a patient's complete medical history from various sources, offering a more comprehensive view.
Quick response to emergencies:
Emergency rooms frequently handle cases with critical time constraints, and having quick access to the most current patient records is immensely beneficial. Swift access to complete patient records enables ER physicians to deliver more effective treatment to patients.
Expedited Pre-Authorizations:
Epic EHR Integration with other health systems streamlines and accelerates the approval process for medical procedures. Epic integration services lead to reduced waiting times for surgeries and operations, minimizing the risk of claim denials for healthcare providers.
Enhanced Accuracy in Diagnosing:
Incomplete patient data can lead to misdiagnosis and subsequent errors in treatment. However, the Epic EMR system consolidates extensive medical information about patients, empowering doctors to make well-informed decisions and improve diagnostic accuracy.
What are the common challenges experienced with the Epic integration process?
- Technical difficulties included creating APIs to enable data sharing across applications with various technology backends.
- Getting multiple parties, such as payers, medical software developers, and organizations, to agree on interoperability.
- HIPAA compliance is ensured by operational processes.
- Legacy interoperability.
What best practices ensure successful Epic integration?
- Develop a clear integration roadmap that aligns with stakeholders' objectives.
- Establish a knowledge base or ensure proficiency among relevant software professionals.
- Set achievable timelines and stick to them.
- Guarantee data security and privacy for the integrated system.
- Maintain operational transparency throughout the integration process.
- Provide comprehensive training for both staff and other users.
Conclusion:
EPIC Integration with various EPIC modules enables mobile accessibility to precise and comprehensive patient records. Custom healthcare software solution developers can enhance Epic EMR integration capabilities for healthcare providers, offering a consolidated view of patient-centric content, including DICOM images.
Healthcare organizations can greatly benefit from such integration, empowering providers and staff with access to information anytime and anywhere.



